In an evolving health landscape, emerging research continues to highlight concerns that could impact everyday wellbeing. Here’s the key update you should know about:
A new ACC scientific statement shows that cholesterol control alone is not enough; targeting inflammation with lifestyle and proven therapies can reduce hidden cardiovascular risk and save lives.
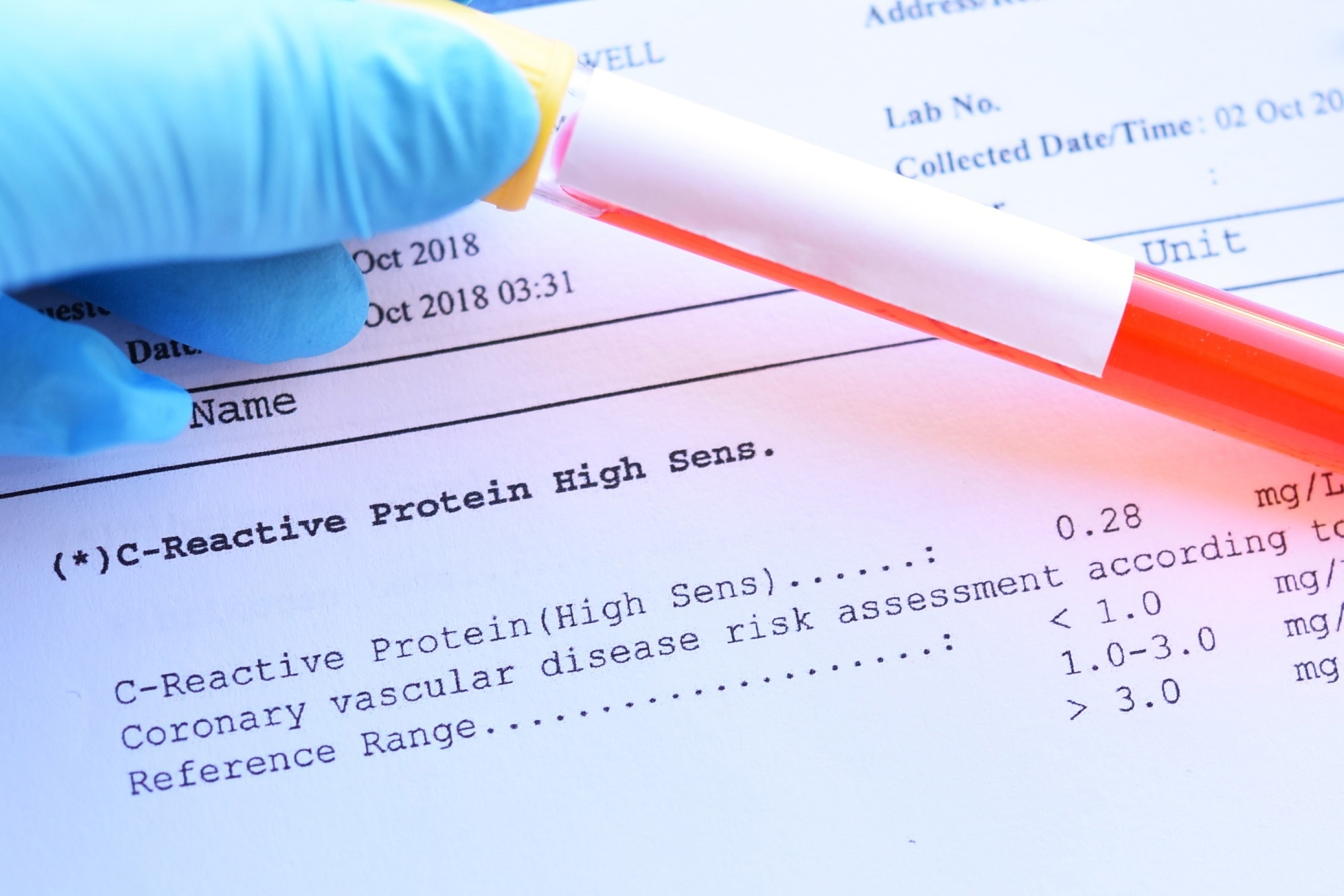
Inflammation and Cardiovascular Disease: 2025 ACC Scientific Statement: A Report of the American College of Cardiology. Image Credit: Jarun Ontakrai / Shutterstock
In a recent Scientific Statement published in the Journal of the American College of Cardiology, a group of authors synthesized evidence on inflammation in cardiovascular disease, defined the use of high-sensitivity C-reactive protein (hsCRP), and outlined practical anti-inflammatory strategies for prevention.
Background
Why do some people still have heart attacks after perfect cholesterol checkups? A growing body of evidence suggests that chronic, low-grade inflammation plays a significant role in driving atherosclerosis, plaque rupture, myocardial infarction (MI), and poor outcomes, even when low-density lipoprotein (LDL) cholesterol levels are controlled. hsCRP captures this “residual inflammatory risk,” identifying individuals who benefit from statins and targeted anti-inflammatory therapy.
Lifestyle patterns, environmental exposures, and coexisting conditions all modulate the inflammatory tone throughout the lifespan. Even as clinical practice adopts biology-based risk assessment, uncertainties persist regarding biomarker panels, imaging markers, and optimal therapies across diverse settings, warranting further research to close these gaps.
Why Inflammation Matters in the Heart
Inflammation orchestrates the entire progression of atherosclerosis, from endothelial dysfunction and the entry of white blood cells into the arterial wall to foam cell formation, plaque progression, rupture, and thrombosis.
Cytokines and chemokines amplify these steps, while impaired clearance of dying cells (efferocytosis) sustains smoldering injury. This “residual inflammatory risk” persists even when LDL cholesterol is on target, which is why patients with excellent lipids can still have heart attacks if inflammation remains unchecked. hsCRP, a stable and widely available blood biomarker, captures this biology in a manner that is easily applicable in the clinic.
hsCRP Belongs Next to Cholesterol, Routinely
Across cohorts and trials, hsCRP predicts cardiovascular events, rivaling or exceeding LDL cholesterol. Cut points of <1, 1–3, and >3 mg/L denote low, average, and high risk, respectively, with other factors. Because concentrations greater than 10 mg/L can reflect intercurrent illness, repeat the test in two to three weeks and use the lower value. After statins, hsCRP >2 mg/L signals residual risk even with LDL <70 mg/dL. The Statement endorses universal hsCRP screening in clinically stable patients for both primary and secondary prevention, alongside LDL-C and Lp(a).
Primary Prevention: Find the “Standard Modifiable Risk Factors (SMuRFs)-less but Inflamed”
In apparently healthy adults, higher hsCRP predicts MI and stroke independent of traditional risks. Some without SMuRFs, like no smoking, diabetes, hypertension, or high LDL cholesterol, still show elevated hsCRP and risk.
First line of lifestyle: improve diet quality, prioritize fruits, legumes, and grains, use olive oil, limit refined carbs and processed meats, engage in 150 minutes per week of moderate (or 75 minutes of vigorous) activity, quit smoking, and lose weight. If hsCRP persists, consider statins despite normal LDL; evidence from the JUPITER trial supports this approach. Primary-prevention anti-inflammatory trials remain needed.
Secondary Prevention: Add Targeted Anti-Inflammation to Guideline Therapy
In established atherosclerotic disease, hsCRP marks residual risk despite care. Interleukin-1 beta (IL-1β) inhibition reduced recurrent events without altering LDL cholesterol; however, it is not approved for cardiovascular use.
Practically, low-dose colchicine 0.5 mg, now FDA-approved for reducing ASCVD events, cuts events by about 25 percent in trials. Start only in clinically stable patients, not during ST-elevation myocardial infarction (STEMI).
Avoid use in patients with hepatic or renal impairment; pause use with cytochrome P450 3A4 (CYP3A4) or P-glycoprotein (P-gp) inhibitors. If hsCRP >2 mg/L on statins, intensify therapy regardless of LDL. IL-6 inhibitors are being tested in chronic kidney disease (CKD), heart failure with preserved ejection fraction (HFpEF), dialysis, and acute coronary syndromes (ACS).
Lifestyle And Behavioral Levers: Food Patterns, Omega-3s, Movement, And Tobacco
Dietary patterns with anti-inflammatory profiles, Mediterranean and Dietary Approaches to Stop Hypertension (DASH), lower systemic inflammation, and reduce events. A simple, memorable prescription: emphasize plants (fruits, vegetables, legumes, whole grains, nuts), prioritize extra-virgin olive oil, eat two to three fish meals per week (favor fatty fish rich in eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]), and minimize refined carbohydrates, red/processed meats, and sugary drinks.
Higher circulating EPA and DHA are associated with lower cardiovascular and all-cause mortality, potentially via specialized pro-resolving mediators (SPMs) that actively terminate inflammation and promote the clearance of inflammatory debris. Regular exercise lowers hsCRP through multiple mechanisms (adipose and skeletal-muscle cytokine shifts, endothelial benefits, metabolic improvements) and is associated with fewer events. Smoking powerfully inflames; quitting restores pro-resolving biology and lowers risk.
Imaging Biomarkers: Promising, Not Yet for Routine Care
Noninvasive imaging techniques, such as computed tomography, magnetic resonance imaging, ultrasound, and positron-emission tomography, can visualize inflamed plaques or inflamed perivascular fat.
The perivascular fat attenuation index (FAI) predicts cardiovascular events independently of coronary artery calcium (CAC) scoring. Still, the Statement advises against the routine use of these imaging biomarkers in everyday practice until stronger clinical utility data and integration frameworks are established. Calcium scoring remains excellent for detecting subclinical atherosclerosis and deciding who to treat; hsCRP helps decide what adjuncts to use.
Inflammation Beyond Arteries: HF and Pericarditis
Heart failure (HF) involves chronic innate-adaptive “parainflammation.” Elevated hsCRP and IL-6 predict worse outcomes, especially in HFpEF. Most anti-cytokine trials have been neutral, though signals remain. Immunosuppression improved inflammatory cardiomyopathy remodeling; omega-3 polyunsaturated fatty acids ≈1 g/day EPA + DHA reduced mortality/hospitalization across New York Heart Association (NYHA) II–IV HF; IL-1β inhibition lowered post-MI HF admissions.
Ongoing IL-6 trials target high hsCRP HFpEF. Recurrent pericarditis: nonsteroidal anti-inflammatory drugs (NSAIDs) plus three months of colchicine halve recurrence. With relapses, IL-1 blockade, such as anakinra or rilonacept, reduces episodes after tuberculosis exclusion.
Inflammation is not a bystander in cardiovascular disease; it is a modifiable driver of risk before and after events. Measuring hsCRP in stable patients provides practical and prognostic insight comparable to traditional factors, revealing who requires more than just lipid-lowering.
Clinicians should pair lifestyle counseling with statins when hsCRP is persistently high and consider low-dose colchicine, now FDA-approved, for stable atherosclerosis under appropriate safety checks.
As trials of IL-6 inhibition and other targeted approaches yield results, personalized strategies will become sharper. Acting now on measurable inflammation can prevent hospitalizations, extend healthy years, and help families plan with confidence.
Journal reference:
- Mensah, G. A., Arnold, N., Prabhu, S. D., Ridker, P. M., & Welty, F. K. (2025). Inflammation and Cardiovascular Disease: 2025 ACC Scientific Statement: A Report of the American College of Cardiology. Journal of the American College of Cardiology. DOI: 10.1016/j.jacc.2025.08.047 https://www.jacc.org/doi/10.1016/j.jacc.2025.08.047

